SEPTEMBER 19, 2016
How DNA Testing Has Changed
1920s – Blood Typing
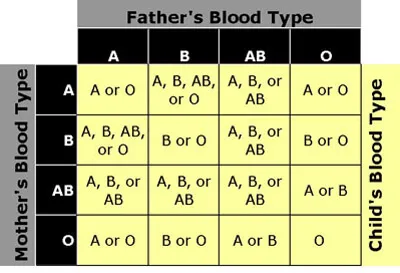
In the early 1900s, scientists identified 4 different blood types in humans – A, AB, B, and O – based on the presence of certain proteins called antigens in the blood. This blood typing system, called the ABO system, provided doctors with crucial information about their patients, allowing them to safely perform medical procedures, especially blood transfusions, by matching the blood types of patients and donors.
In the 1920s, scientists recognized that blood types were genetically inherited. A blood typing chart, shown below, was developed to show the relationship between parents and their children.
Scientists realized that they could predict the blood type of a child based on his/her parents’ blood types. Conversely, if one of the parents’ blood types was unknown, the scientist could use the blood types of the child and the known parent to identify the missing parent’s blood type. In this way, scientists used blood typing to determine paternity or maternity of a child. However, because the information from blood typing is limited, it was difficult to definitively identify biological relationships.
For example, if a child had Type A blood and the child’s mother had Type AB blood, the child’s biological father could have any of the 4 blood types. This means that based on blood typing alone, no man could be excluded as the child’s father.
In the end, the power of exclusion (the power of a test to eliminate a certain percentage of the population from being biologically related to an individual) for blood testing is only 30%. Blood typing is not a useful technique for determining paternity.
1930s – Serological Testing
In the 1930s, scientists discovered other proteins in the blood that could be used for identifying humans. The Rh, Kell, and Duffy blood group systems, like the ABO system, were based on the presence of specific antigens in the blood. These antigens are also genetically inherited, proving useful in identifying possible biological relationships.
Through these serological tests, scientists could use the blood group systems of two parents to predict the possible blood group of their child. Scientists also applied serological testing to paternity cases, attempting to identify alleged fathers based on the blood groups of the child and mother. However, much like the use of the ABO system for paternity testing, serological tests are not conclusive in identifying biological parents. The power of exclusion for serological testing is only 40%, meaning this technique is not effective in identifying biological relationships.
1970s – HLA Testing
In the mid 1970s, scientists turned from blood typing to tissue typing. Scientists discovered the human leukocyte antigen (HLA), a protein prevalent in all of the body except the red blood cells. White blood cells in particular carry a high concentration of HLA. There are many different types of HLA, and these types vary between each person. Because of the high variability of HLA types between different people, HLA testing became a more powerful mode of paternity testing. The power of exclusion for HLA testing alone is 80% and coupled with blood typing and serological testing is close 90%.
Despite its more powerful ability to identify biological relationships, HLA testing is not an ideal technique. HLA testing requires a large blood sample that must be no older than a few days old. The collection process can be uncomfortable, making it dangerous for infants under the age of 6 months.
1980s – DNA Testing Using RFLP Technique
In the mid 1980s, a technique was developed called restriction fragment length polymorphism (RFLP, pronounced “rif-lip”). This technique became the first genetic test using DNA. Like HLA and blood proteins, DNA is genetically inherited from both parents. However, sections of DNA are highly variable and more unique than HLA and blood proteins, and it is found in every part of the body. These attributes make DNA ideal for identifying biological relationships.
RFLP allows scientists to cut out the unique sections of the DNA, which is extracted from blood samples. For paternity testing, these unique sections of the parents and child are compared. Half of the child’s DNA should match the mother’s DNA, and half should match the father’s DNA if they are biologically related.
Sometimes during this procedure, the child’s DNA will not appear to match either parent’s DNA, possibly caused bygenetic mutations. When this occurs, scientists will perform statistical analysis to determine the possibilities of mutation and biological relationship between family members.
Because RFLP is applied to DNA testing, this procedure yields highly conclusive results, typically with a power of exclusion higher than 99.99%. However, this technique is not performed frequently today because, like HLA testing, RFLP requires a large blood sample and a longer turnaround time.
1990s – DNA Testing Using PCR Technology
Although developed in the 1980s, polymerase chain reaction (PCR) technique in DNA testing became the standard process for paternity testing in the 1990s.
PCR is a technique through which samples of DNA fragments are copied and replicated many times until billions of copies are made. Because of the power of PCR, very small samples of DNA from any part of the body can be used in a DNA test. Additionally, the process is quick.
By using PCR technology in DNA testing, paternity and other DNA tests can be performed much more easily and quickly. In a standard paternity test, DNA samples will be painlessly collected through buccal swabs from the mother, child, and alleged father. Then, the samples will be replicated through PCR and compared for similarities. Because half of the child’s DNA is inherited from the mother and the other half from the father, the child’s DNA should match portions of both biological parents.
Because DNA is being tested in this process, results yielded from a paternity test using PCR technology are often higher than 99.99%. This process has become the standard for biological identification, as it requires only a small sample from any person (even in prenatal cases), is highly conclusive, and provides results very quickly.
About DNA Diagnostics Center (DDC)
DNA Diagnostic Center is the world leader in paternity and relationship testing. We serve healthcare professionals, government agencies, and individuals around the world to determine family relationships with trusted accuracy.
More Questions? Don’t hesitate to call us: we’re here to help!
CALL NOW